It’s World Kidney Day. Not a day that I’d ever heard of (until actually today, in fact). And not a day I’d normally pay much attention to, except that in early February, I donated a kidney to my friend, Jen.
I haven’t talked about it publicly (READ: on social media) because I don’t super like being a focus of attention and for a long time – several months – it wasn’t even clear if I would be able to donate.
After I had donated and it was all said and done, another friend of mine, Dustin, who donated a kidney a decade or so ago said, tongue firmly in cheek, “You sick of being called a hero yet?” And … yeah. I kinda was.
But I get it.
Surgery is a big deal. Elective surgery doubly so. People don’t understand the donation process. The most anyone has probably thought about it is the urban legend of waking up in a bathtub full of ice with a dire note ‘ur kidn3y5 hav3 b33n r3m0v3d, ca11 911.’
But it also made me think about the process of deciding to go through with it and, looking back, the biggest factor in giving me a measure of comfort and confidence in the process was talking with my friend Dustin. He talked frankly with me about how it went. Answered my questions.
And, listen, the patient advocates at UCLA are terrific. They gave me a lot of information, provided resources, answered questions, and certainly want positive outcomes from every donation, so they’re not cutting corners or holding anything back… but it was different coming from a friend.
Talking with Dustin gave me confidence that I could do it. In a different way than talking with the UCLA staff.
So, if I can be that friend to folks in my reach, I will be.
WHO (did you donate to?): I donated to the aforementioned Jen, who at the start of this had been on dialysis 3 times a week for two years.
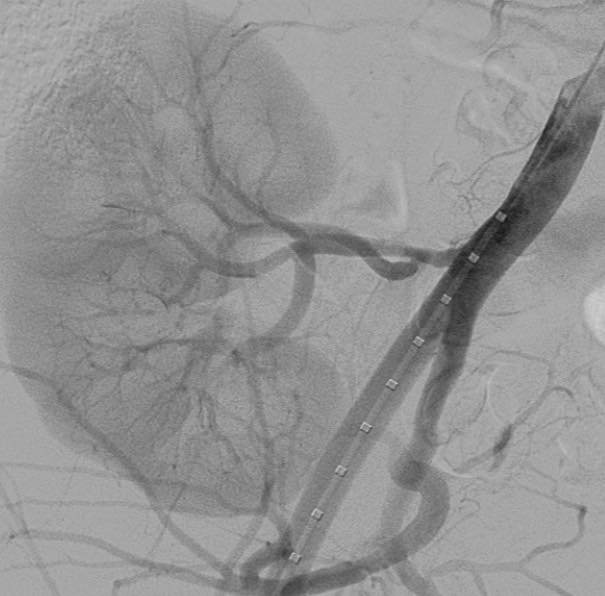
WHAT (did you donate?): My left kidney, which I learned is the preferred kidney if both have equal function (longer connective bits for surgeons to work with).
WHAT II (was the procedure?): a laparoscopic nephrectomy; laparoscopic (make 3 small incisions less than 1/2 each, one for a scope that is the surgeon’s eyes, one for a tool rig that is the surgeon’s hands, and one for the gas to inflate); nephr (kidney) ectomy (remove it) which required an incision of 3-4 inches long across my abdomen below my belly button; there is a lot more fascinating about the whole procedure that is more than I care to type, but it’s really pretty incredible — one small thing, the recipient doesn’t have a kidney removed to have one installed, they get a third kidney!
WHEN (did all this go down?): The process started in May of 2023, with medical and psychological evaluations through the Summer, and a decision to go ahead in early Fall; surgery was scheduled for early February 2024.
WHERE (did it go down?): tests at various Qwest Diagnostic centers and UCLA Medical Plaza; evals on video calls and at UCLA’s Connie Frank Kidney Transplant Center; surgery at Ronald Reagan UCLA Medical Center.
WHY (did you do it?): Jen is cool and dialysis sucks; the waiting list for a kidney from a deceased donor in California is 10 years; plus, kidneys from living donors have a significantly higher success rate.
HOW (much did all this cost you?): $0.00 I have no idea how much it cost. The testing was definitely over $3000 and I paid $0.00 for it; the NLDAC provided substantial additional support to make sure the process did not have a financial impact on me (including meal stipends and lodging for caregivers, and even airfare, fuel, and future checkup visits are supported); none of the visits or procedures cost me anything.
SCREENING AND THE LEAD UP
There were ONE MILLION tests. I had a lot of blood drawn and gave many samples along the way; a couple weeks before the surgery SEVENTEEN vials in one sitting. Big ups to the phlebotomists at UCLA’s Medical Plaza.

Via those tests, I learned a lot about my health. It’s good! One of the surgeons said ‘your chart is really boring, we love it.’ Detailed medical knowledge is good to have. ALSO: the experience of getting contrast for CT scan is TRIPPY and cool and now I have a badass 3D scan of my entire torso.
The point of all these tests is not just to learn about my kidney function, definitely that, but also if I was healthy enough to donate. It’s a surgery that leaves you poorer on purpose and it’s important to determine if that was going to be okay for me.
There were a lot of conversations. I had a dedicated RN (Max) who coordinated oversaw the whole process and answers my questions, a designated logistics coordinator (Jen, different Jen) who got me information, test materials, parking and lunch vouchers; surgeons checking in (Eric) going over the surgery and my scan; a social worker (Mara) who helped really ground what it meant to do this, long term health implications, lifestyle changes, nutrition, and more; nephrologists… a lot of people looking out for my personal well-being throughout the process.
And all along the way, assurance that it was okay to stop for any reason.
SURGERY AND THE DAY AFTER
The Ronald Reagan UCLA Medical Center is MASSIVE. And that might make it feel faceless and clinical, but it was a very human and very well-organized experience all around. Talk to my sweetie, Kevin, and my mom about the caretaker experience, they have a really different lens to view this all through, mostly ‘wow, this is pretty incredible.’ Which… agreed.
I stayed at a hotel near the hospital (paid for by NLDAC) and went in at 5am. It’s a bit of a blur. There was a parade of healthcare professionals, nurses, surgeons, doing pre-op. The anesthetist is the last person I spoke to before going under (no surprise). Surgery took a couple hours. I have sketchy memories of waking up and Jen and I joked that we wished we could have adjoining surgical suites so we could high-5 from our gurneys as the kidney was relayed. AS IT HAPPENS, I was leaving Recovery pretty much just as she was arriving and I got wheel past her bed — and we got to air-5 each other — and though I didn’t hear it, Kevin said that Jen’s nurse was holding up a bag and talking about Jen’s kidney (hers now! <3) was already producing urine. As fast as that. Incredible.
The next 24 hours is a definite blur. I spent a good day on a non-narcotic IV drip that smoothed out the worst of discomfort. I asked for morphine once. It burns going in, that surprised me. Not much, though, and the RN does the equivalent of the dentist wiggling your cheek through the process.
I was up and walking by ~7pm that night. I didn’t go far and got a little woozy. Getting up was the hardest part of the process.
Liquid meals. Pudding, popsicles, broth, juice. Not satisfying, but better than the nothing I’d had before the surgery. My mom stayed with my in my room the whole day and through the night (bless her heart) and I recommend having someone there if you can. It was definitely reassuring. Though the nurses were incredibly responsive when I hit the call button. Kevin was back and forth across town (45-to 75 minute trips) taking care of business, work home, and more – that they could tagteam was handy.
I talked to my BFF Katy on the phone who had me laughing (ow ow ow) at all the ‘adventures my kidney was going to have’ and contributed the title of this blog which I am still laughing at.
I also talked to Jen which was really great.
The next day was another parade of specialists, dieticians, social worker (Mara again <3), one of the surgeons; I was discharged after lunch (I had a grilled cheese and tomato soup, it was good!) after the surgical team signed off and went up to see Jen who was doing awesome. She looked better and was in good spirits.
RECOVERY AT HOME
For a week I was pretty tender. And the first night had some unhappy moments where I realized I needed to get up but really couldn’t. That’s where help came in (thank you, sweetie). I worked out a way to carefully get my center of mass such that I didn’t have to engage my belly to sit up, so by day 2 I was able to get in and out of bed on my own. Walking was encouraged.
The second week was better. And the third better still.
It’s a little over 5 weeks out now and I can still feel a bit of a twinge in certain movements, but I am mostly recovered.
Jen is doing well. It took a bit to get meds and kidney totally settled in, but she’s a great patient and the doctors are pleased.
THE FUTURE
I have checkups at 6 months and 1 year. If I ever end up in need of a kidney, a donor has priority on available kidneys, which I didn’t think about, but is actually kinda nice.
Dietary considerations are the ‘biggest’ change to things for me. I now have MORE reason to eat healthfully, though if I ever want to get yoked it’ll be a struggle because I can’t pound protein like a 2-kidney person. I need to keep an eye on my blood pressure which is good so far. And also watch the use of NSAIDs (pain killers like Advil and Aleve) because they’re rough on kidneys.
But that’s that. The whole process was fascinating, informative, somewhat uncomfortable in the doing, but totally manageable. I have a good support system and … you probably have one too, people came OUT OF THE WOODWORK with offers of support and help and encouragement.
If you have any questions, just holler.
UCLA Kidney Transplant Center
National Living Donor Assistance Center


Karen!! This is Max. Thanks for sharing this. So happy that I got to be a part of your journey. This warms my heart.
Right back, Max. ^_^ Thanks for being there.